Keywords
Abstract
Purpose: Rigorous clinical testing has established that Schlemm’s canal cross-sectional area (SC-CSA) is reduced in glaucomatous eyes. However, to date, it is unclear whether trabecular bypass procedures impact the morphology of the proximal aqueous outflow tract, or if the introduction of a local region of low outflow resistance adversely affects SC-CSA elsewhere, specifically presenting as SC diminution. This study quantifies changes in the morphology of the distal outflow pathway after iStent Trabecular Micro-Bypass stent (Glaukos Corp, Laguna Hills, CA, USA) implantation in living eyes by anterior segment optical coherence tomography (OCT).
Design: This was a prospective observational study.
Subjects: This study included six patients (eight eyes) with primary-open angle glaucoma.
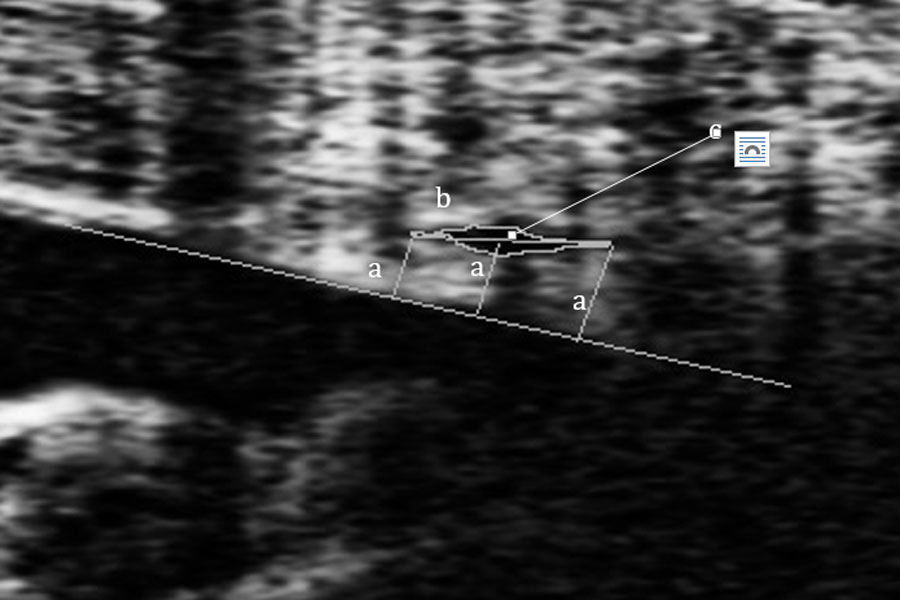
Methods: Patients underwent iStent placement in the nasal anterior chamber angle quadrant. OCT imaging was obtained of both nasal and temporal eye quadrants before and after surgery. For each SC parameter, an average of ten consecutive, evenly spaced measurements were manually obtained over a 1 mm segment of SC on FIJI ImageJ. Linear mixed effects modeling quantified the effect of the iStent on these parameters.
Main outcome measures: Main outcome measures were changes in SC-CSA, inner-to-outer wall distance (IOD), and trabecular meshwork (TM) thickness following iStent placement.
Results: Following iStent placement, total SC-CSA increased an average of 1,039.12 μm2 (P = 0.05). Individually, there were no significant changes in SC-CSA in the nasal or temporal quadrants. Total SC-IOD and nasal SC-IOD increased an average of 2.35 μm (P = 0.01) and 2.96 μm (P = 0.04), respectively. There were no significant changes in temporal quadrant SC-IOD. There were no significant changes in TM thickness in either quadrant.
Conclusions: Implantation of the iStent Trabecular Micro-Bypass stent significantly increases SC-IOD in the nasal quadrant at the location of implant, with no evidence of SC diminution in the temporal quadrant. It remains unclear how these observations relate to the surgical efficacy of trabecular bypass procedures.
References
Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262-267.
Sommer A, Tielsch JM, Katz J, et al. Racial differences in the cause-specific prevalence of blindness in east Baltimore. N Engl J Med. 1991;325(20):1412-1417.
Sommer A, Tielsch JM, Katz J, et al. Relationship between intraocular pressure and primary open-angle glaucoma among white and black Americans. The Baltimore Eye Survey. Arch Ophthalmol. 1991;109(8):1090-1095.
Mitchell P, Lee AJ, Rochtchina E, Wang JJ. Open-angle glaucoma and systemic hypertension: the Blue Mountains Eye Study. J Glaucoma. 2004;13(4):319-326.
Leske MC, Wu SY, Hennis A, Honkanen R, Nemesure B. Risk factors for incident open-angle glaucoma: the Barbados Eye Studies. Ophthalmology. 2008;115(1):85-93.
Leske MC, Connell AM, Wu SY, Hyman L, Schachat AP. Distribution of intraocular pressure. The Barbados Eye Study. Arch Ophthalmol. 1997;115(8):1051-1057.
Mitchell P, Smith W, Attebo K, Healey PR. Prevalence of open-angle glaucoma in Australia. The Blue Mountains Eye Study. Ophthalmology. 1996;103(10):1661-1669.
Gabelt BK, P. Adler’s Physiology of the Eye. St. Louis, MO: Mosby; 2003.
Tamm ER. The trabecular meshwork outflow pathways: structural and functional aspects. Exp Eye Res. 2009;88(4):648-655.
Hong J, Xu J, Wei A, et al. Spectral-domain optical coherence tomographic assessment of Schlemm’s canal in Chinese subjects with primary open-angle glaucoma. Ophthalmology. 2013;120(4):709-715.
Grant WM. Experimental aqueous perfusion in enucleated human eyes. Arch Ophthalmol. 1963;69:783-801.
Jocson VL, Sears ML. Experimental aqueous perfusion in enucleated human eyes. Results after obstruction of Schlemm’s canal. Arch Ophthalmol. 1971;86(1):65-71.
Ahmed, II, Katz LJ, Chang DF, et al. Prospective evaluation of microinvasive glaucoma surgery with trabecular microbypass stents and prostaglandin in open-angle glaucoma. J Cataract Refract Surg. 2014;40(8):1295-1300.
Arriola-Villalobos P, Martinez-de-la-Casa JM, Diaz-Valle D, Fernandez-Perez C, Garcia-Sanchez J, Garcia-Feijoo J. Combined iStent trabecular micro-bypass stent implantation and phacoemulsification for coexistent open-angle glaucoma and cataract: a long-term study. Br J Ophthalmol. 2012;96(5):645-649.
Fea AM. Phacoemulsification versus phacoemulsification with micro-bypass stent implantation in primary open-angle glaucoma: randomized double-masked clinical trial. J Cataract Refract Surg. 2010;36(3):407-412.
Fea AM, Belda JI, Rekas M, et al. Prospective unmasked randomized evaluation of the iStent inject ((R)) versus two ocular hypotensive agents in patients with primary open-angle glaucoma. Clin Ophthalmol. 2014;8:875-882.
Samuelson TW, Katz LJ, Wells JM, Duh YJ, Giamporcaro JE. Randomized evaluation of the trabecular micro-bypass stent with phacoemulsification in patients with glaucoma and cataract. Ophthalmology. 2011;118(3):459-467.
Spiegel D, Wetzel W, Neuhann T, et al. Coexistent primary open-angle glaucoma and cataract: interim analysis of a trabecular micro-bypass stent and concurrent cataract surgery. Eur J Ophthalmol. 2009;19(3):393-399.
Kagemann L, Wang B, Wollstein G, et al. IOP elevation reduces Schlemm’s canal cross-sectional area. Invest Ophthalmol Vis Sci. 2014;55(3):1805-1809.
Kagemann L, Wollstein G, Ishikawa H, et al. Identification and assessment of Schlemm’s canal by spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2010;51(8):4054-4059.
Kagemann L, Wollstein G, Ishikawa H, et al. 3D visualization of aqueous humor outflow structures in-situ in humans. Exp Eye Res. 2011;93(3):308-315.
Hong J, Yang Y, Wei A, et al. Schlemm’s canal expands after trabeculectomy in patients with primary angle-closure glaucoma. Invest Ophthalmol Vis Sci. 2014;55(9):5637-5642.
Wang F, Shi G, Li X, et al. Comparison of Schlemm’s canal’s biological parameters in primary open-angle glaucoma and normal human eyes with swept source optical. J Biomed Opt. 2012;17(11):116008.
Hammer D, Ferguson RD, Iftimia N, et al. Advanced scanning methods with tracking optical coherence tomography. Opt Express. 2005;13(20):7937-7947.
Dietlein TS, Jacobi PC, Luke C, Krieglstein GK. Morphological variability of the trabecular meshwork in glaucoma patients: implications for non-perforating glaucoma surgery. Br J Ophthalmol. 2000;84(12):1354-1359.
Bahler CK, Smedley GT, Zhou J, Johnson DH. Trabecular bypass stents decrease intraocular pressure in cultured human anterior segments. Am J Ophthalmol. 2004;138(6):988-994.
Fernandez-Barrientos Y, Garcia-Feijoo J, Martinez-de-la-Casa JM, Pablo LE, Fernandez-Perez C, Garcia Sanchez J. Fluorophotometric study of the effect of the glaukos trabecular microbypass stent on aqueous humor dynamics. Invest Ophthalmol Vis Sci. 2010;51(7):3327-3332.
Yuan F, Schieber AT, Camras LJ, Harasymowycz PJ, Herndon LW, Allingham RR. Mathematical Modeling of Outflow Facility Increase With Trabecular Meshwork Bypass and Schlemm Canal Dilation. J Glaucoma. 2015.
Gillmann K, Bravetti GE, Mansouri K, Mermoud A. Anterior Segment Optical Coherence Tomography Signs of Local Dilatation Effect of a Micro-Stent on Schlemm’s Canal. Nepal J Ophthalmol. 2018;10(20):184-187.
Huang AS, Penteado RC, Papoyan V, Voskanyan L, Weinreb RN. Aqueous Angiographic Outflow Improvement after Trabecular Microbypass in Glaucoma Patients. Ophthalmol Glaucoma. 2019;2(1):11-21
Tamm ER, Braunger BM, Fuchshofer R. Intraocular Pressure and the Mechanisms Involved in Resistance of the Aqueous Humor Flow in the Trabecular Meshwork Outflow Pathways. Prog Mol Biol Transl Sci. 2015;134:301-314.
de Kater AW, Spurr-Michaud SJ, Gipson IK. Localization of smooth muscle myosin-containing cells in the aqueous outflow pathway. Invest Ophthalmol Vis Sci. 1990;31(2):347-353.
Kagemann L, Nevins JE, Jan NJ, et al. Characterisation of Schlemm’s canal cross-sectional area. Br J Ophthalmol. 2014;98 Suppl 2:ii10-14.