Keywords
Abstract
Purpose: Several elements are developed to quantitatively determine the contribution of different physical and chemical effects to tear breakup (TBU) in subjects with no self-reported history of dry eye (DED) or other ocular surface disease. Fluorescence (FL) imaging is employed to visualize the tear film (TF) and to determine TF thinning and potential TBU.
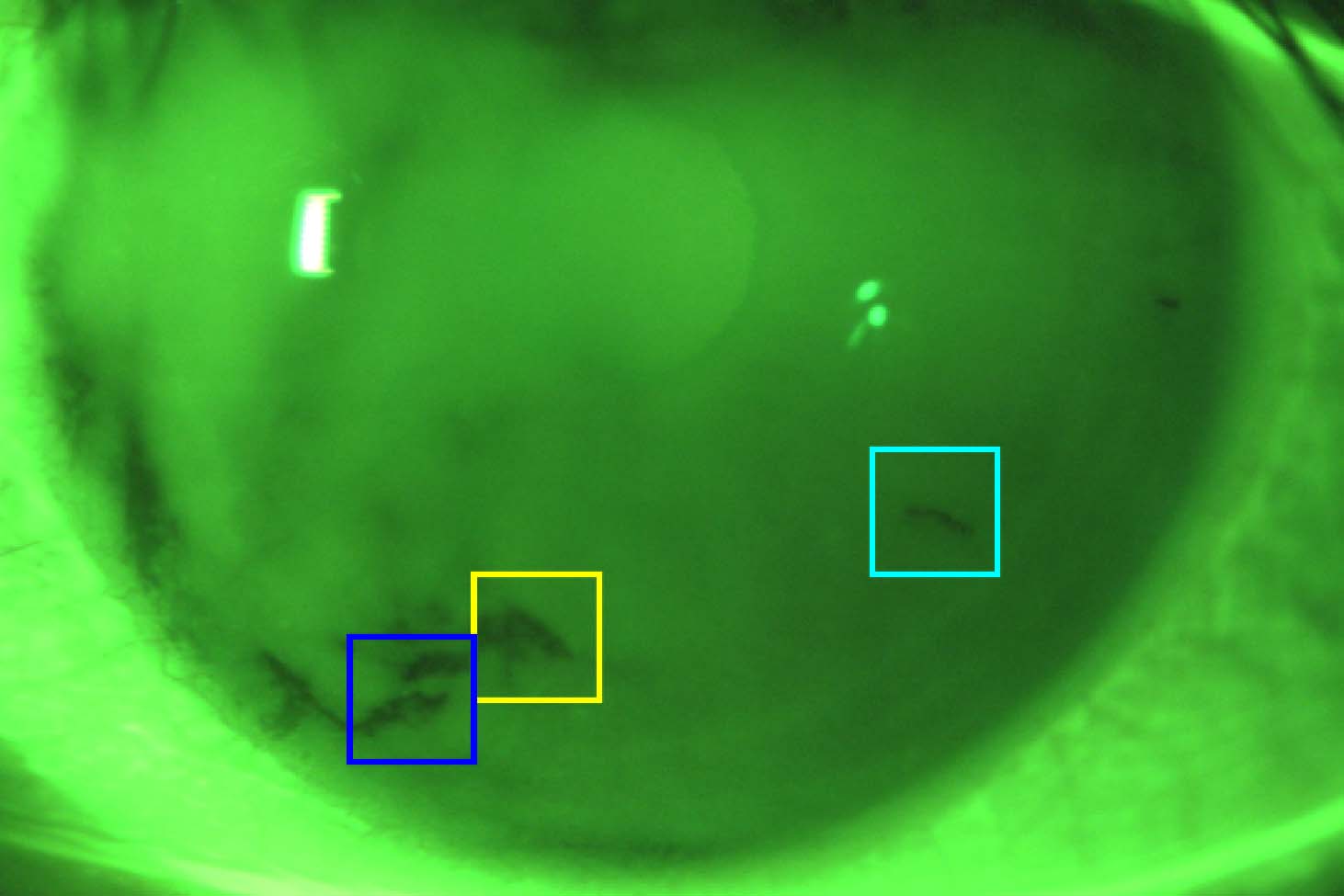
Methods: An automated system using a convolutional neural network that was trained and tested on more than 50,000 images from FL imaging experiments was deployed. The trained system could identify multiple TBU instances in each trial. Once identified, extracted FL intensity data was fit by mathematical models that included tangential flow along the eye, evaporation, osmosis, and FL intensity of emission from the TF. The mathematical models consisted of systems of ordinary differential equations for the aqueous layer thickness, osmolarity, and the FL concentration; they are a local approximation to TF thinning and/or TBU dynamics. FL intensity was computed using the resulting thickness and FL concentration. Optimizing the fit of the models to the FL intensity data determined the mechanism(s) driving each instance of TBU and produced an estimate of the osmolarity within TBU.
Results: Initial estimates for FL concentration and initial TF thickness agree well with prior results. Fits were produced for N = 467 instances of potential TBU from 15 non-DED subjects. The results showed a distribution of causes of TBU in these healthy subjects, as reflected by estimated flow and evaporation rates, which appear to agree well with previously published data. Final osmolarity depended strongly on the TBU mechanism, generally increasing with evaporation rate but complicated by the dependence on flow.
Conclusion: The method has the potential to classify TBU instances based on the mechanism and dynamics, and to estimate the final osmolarity at the TBU locus. The results suggest that it might be possible to classify individual subjects and provide a baseline for comparison and potential classification of DED subjects.
References
Schaumberg DA, Dana R, Buring JE, Sullivan DA. Prevalence of dry eye syndrome among USwomen. Am. J. Ophthalmol. 2003; 318–326.
Schaumberg DA, Dana R, Buring JE, Sullivan DA. Prevalence of dry eye disease among US men: estimates from the Physicians’ Health Studies. Arch. Ophthalmol. 2009;127, 763–768.
Stapleton F, Garrett Q, Chan C, Craig JP. The Epidemiology of Dry Eye Disease. Dry Eye. Berlin: Springer, 2015; chap. 2, 21–29.
Stapleton F, Alves M, Bunya VY, Jalbert I, Lekhanont K, Malet F, et al. TFOS DEWS II Epidemiology Report. Ocul. Surf. 2017;15(3): TFOS International Dry Eye WorkShop (DEWS II), 334–365. Available from: https://www.sciencedirect.com/science/article/pii/S154201241730109X. doi: https://doi.org/10.1016/j.jtos.2017.05.003.
Nelson JD, Craig JP, Akpek EK, Azar DT, Belmonte C, Bron AJ, et al. TFOS DEWS-II Introduction. Ocul. Surf. 2017;15(3): 269–275.
Pult H, Tosatti S, Spencer ND, Asfour JM, Ebenhoch M, Murphy PJ. Spontaneous Blinking from a Tribological Viewpoint. Ocul. Surf. 2015;13(3): 236–249. doi: 10/f7h7rb.
Thibos LN, Hong X. Clinical Applications of the Shack-Hartmann Aberrometer. Optom. Vis. Sci. 1999;76(12): 817–825. doi: 10.1097/00006324-199912000-00016.
Norn MS. Desiccation of the Precorneal Film. Acta Ophthalmol, 1969;47(4): 881–889. doi: 10/dj95jq.
Cho P, Leung L, Lam A, Choi A. Tear Break-up Time: Clinical Procedures and Their Effects. Ophthal. Physl. Opt. 1998;18(4): 319–324. doi: 10/c3x7pw.
Mapstone R. Measurement of corneal temperature. Exp. Eye Res. 1968;7, 237–242.
Efron N, Young G, Brennan NA. Ocular surface temperature. Curr. Eye. Res. 1989;8, 901–906.
Belmonte C, Gallar J. Cold Thermoreceptors, Unexpected Players in Tear Production and Ocular Dryness Sensations. Invest. Ophthalmol. Vis. Sci. 2011;52(6): 3888–92. doi: 10/ct43xw.
Nichols JJ, Mitchell GL, King-Smith PE. Thinning Rate of the Precorneal and Prelens Tear Films. Invest. Ophthalmol. Vis. Sci. 2005;46(7): 2353–2361. doi: 10/fk2px5.
Dursch TJ, Li W, Taraz B, Lin MC, Radke CJ. Tear-Film Evaporation Rate from Simultaneous Ocular-Surface Temperature and Tear-Breakup Area. Optom Vis Sci, 2018;95, 5–12. doi: https://doi.org/10.1097/OPX.0000000000001156.
Lemp MA et al. The definition and classification of dry eye disease: Report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop. Ocul. Surf. 2007;5, 75–92.
Liu H, Begley CG, Chen M, Bradley A, Bonanno J, McNamara NA, et al. A Link between Tear Instability and Hyperosmolarity in Dry Eye. Invest. Ophthalmol. Vis. Sci. 2009;50, 3671–3679.
Braun RJ, King-Smith PE, Begley CG, Li L, Gewecke NR. Dynamics and function of the tear film in relation to the blink cycle. Prog. Retin. Eye Res. 2015;45, 132–164.
Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, et al. TFOS DEWS II Definition and Classification Report. Ocul. Surf. TFOS International Dry Eye WorkShop (DEWS II), 2017;15(3): 276–283. doi: 10/gbstrp.
Awisi-Gyau D, Begley C, Situ P, Simpson TL. Changes in Corneal Detection Thresholds After Repeated Tear Film Instability. Invest. Ophthalmol. Vis. Sci. 2019;60(13): 4234. doi: 10/ghwn4b.
Wolffsohn JS, Arita R, Chalmers R, Djalilian A, Dogru M, Dumbleton K, et al. TFOS DEWS II Diagnostic Methodology Report. Ocul. Surf. TFOS International Dry Eye WorkShop (DEWS II), 2017;15(3): 539–574. doi: 10/ghtxdd.
Cho P, Brown B, Chan I, Conway R, Yap M. Reliability of the Tear Break-Up Time Technique of Assessing Tear Stability and the Locations of the Tear Break-Up in Hong Kong Chinese: Optom. Vis. Sci. 1992;69(11): 879–885. doi: 10/fb4kjv.
Mengher LS, Bron AJ, Tonge SR, Gilbert DJ. A Non-invasive Instrument for Clinical Assessment of the Pre-corneal Tear Film Stability. Curr. Eye Res. 1 1985;4, 1–7.
Llorens-Quintana C, Szczesna-Iskander D, Iskander DR. A unified approach to tear film surface analysis with high speed videokeratoscopy. J. Opt. Soc. Am. A, 2019;36, B15–B22. doi: 10.1364/JOSAA.36.000B15.
Doane M. An Instrument for in Vivo Tear Film Interferometry. Optom. Vis. Sci. 1989;66, 383–8.
Danjo Y, Nakamura M, Hamano T. Measurement of the human precorneal tear film with a noncontact optical interferometry film thickness measurement system. Jpn. J. Ophthalmol. 1994;38, 260–66.
Goto E, Tseng SC. Kinetic analysis of tear interference images in aqueous tear deficiency dry eye before and after punctal occlusion. Invest. Ophthalmol. Vis. Sci. 2003;44, 1897–1905.
King-Smith PE, Fink BA, Hill RM, Koelling KW, Tiffany JM. The thickness of the tear film. Curr. Eye. Res. 2004;29, 357–368.
Segev F, Geffen N, Galor A, Cohen Y, Gefen R, Belkin A, et al. Dynamic Assessment of the Tear Film Muco-Aqueous and Lipid Layers Using a Novel Tear Film Imager (TFI). Br. J. Ophthalmol. 2020;104(1): 136–141. ISSN: 0007-1161, 1468-2079. doi: 10.1136/bjophthalmol-2018-313379.
King-Smith PE, Reuter KS, Braun RJ, Nichols JJ, Nichols KK. Tear film breakup and structure studied by simultaneous video recording of fluorescence and tear film lipid layer, TFLL, images. Invest. Ophthalmol. Vis. Sci. 2013;54, 4900–4909.
Norn MS. Tear Film Breakup Time: A Review. The Preocular Tear Film in Health, Disease and Contact Lens Wear. Lubbock, TX: Dye Eye Institute, 1986; 52–56.
Vyas AH, Mehta MA. A Comprehensive Survey on Image Modality Based Computerized Dry Eye Disease Detection Techniques. Adv. Sci. Technol. Eng. Sys. J. 2020;5(2): 748–756. doi: 10/ghwn37.
T. Yedidya R. Hartley JG. Automatic Detection of Pre-ocular Tear Film Break-Up Sequence in Dry Eyes. 2008 Digital Image Computing: Techniques and Applications, 2008; 442–448. doi: 10.1109/dicta.2008.70.
Ramos L, Barreira N, Mosquera A, Penedo MG, Yebra-Pimentel E, García-Resúa C. Analysis of Parameters for the Automatic Computation of the Tear Film Break-up Time Test Based on CCLRU Standards. Comp. Meth. Prog. Biomed. 2014;113(3): 715–724. doi: 10/f5tgrc.
Bartuzel MM, Szczesna-Iskander D, Iskander DR. Automatic dynamic tear meniscus measurement in optical coherence tomography. Biomed. Opt. Express, 8 2014;5, 2759–2768. doi: 10.1364/boe.5.002759.
Acharya U, Tan J, Koh J, Sudarshan V, Yeo S, Too C, et al. Automated diagnosis of dry eye using infrared thermography images. Infrared Phys. Techn. 2015;71, 263–271. doi: 10.1016 /j .infrared.2015.04.007.
Su TY, Liu ZY, Chen DY. Tear Film Break-Up Time Measurement Using Deep Convolutional Neural Networks for Screening Dry Eye Disease. IEEE Sensors J. 2018;18(16): 6857–6862. doi: 10.1109/jsen.2018.2850940.
Remeseiro B, Mosquera A, Penedo MG. CASDES: A Computer-Aided System to Support Dry Eye Diagnosis Based on Tear Film Maps. IEEE J. Biomed. Health Inform. 2016;20(3): 936–943. doi:10/ghwn4f.
Gaffney E, Tiffany J, Yokoi N, Bron A. A mass and solute balance model for tear volume and osmolarity in the normal and the dry eye. Prog. Ret. Eye Res. 2010;29, 59–78.
Cerretani CF, Radke CJ. Tear Dynamics in Healthy and Dry Eyes. Curr. Eye Res. 6 2014;39, 580–595. doi: 10.3109/02713683.2013.859274.
Gause S, Hsu KH, Shafor C, Dixon P, Powell KC, Chauhan A. Mechanistic modeling of ophthalmic drug delivery to the anterior chamber by eye drops and contact lenses. Adv. Colloid Interface Sci. 2016;233, 139–154. doi: 10.1016/j.cis.2015.08.002.
Kim YY, Nguyen T, Lin MC, Peng CC, Radke CJ. Protection against corneal hyperosmolarity with soft contact-lens wear. Prog. Ret. Eye Res. 2022;87, 101012. doi: 10.1016/j.preteyeres.2021.101012.
Sharma A, Tiwari S, Khanna R, Tiffany JM. Hydrodynamics of meniscus-induced thinning of the tear film. Advances in Experimental Medicine and Biology. Ed. by DA Sullivan, DA Dartt, MA Meneray. 438. Lacrimal Gland, Tear Film, and Dry Eye Syndromes 2. Berlin: Springer, 1998; 425–431.
Wong H, Fatt I, Radke CJ. Deposition and thinning of the human tear film. J. Colloid Interface Sci. 1996;184, 44–51.
Miller KL, Polse KA, Radke CJ. Black line formation and the “perched” human tear film. Curr. Eye Res. 2002;25, 155–162.
Berger RE, Corrsin S. A surface tension gradient mechanism for driving the pre-corneal tear film after a blink. J. Biomech. 1974;7, 225–238.
Braun RJ, Fitt AD. Modeling the drainage of the precorneal tear film after a blink. Math. Med. Biol. 2003;20, 1–28.
Winter KN, Anderson DM, Braun RJ. A model for wetting and evaporation of a post-blink precorneal tear film. Math. Med. Biol. 2010;27, 211–225.
BraunRJ,Usha R,McFadden GB, Driscoll TA, Cook LP, King-Smith PE. Thin film dynamics on a prolate spheroid with application to the cornea. J. Eng. Math. 2012;73, 121–138. doi: 10.1007/s10665-011-9482-4.
Peng CC, Cerretani C, Braun RJ, Radke CJ. Evaporation-Driven Instability of the Precorneal Tear Film. Adv. Coll. Interface Sci. 2014;206, 250–264.
Braun RJ, Driscoll TA, Begley CG, King-Smith PE, Siddique JI. On Tear Film Breakup (TBU): Dynamics and Imaging. Math. Med. and Biol. 2018;35(2): 145–180. doi: 10.1093/imammb/dqw023.
Zhong L, Braun RJ, Begley CG, King-Smith PE. Dynamics of Fluorescent Imaging for Rapid Tear Thinning. Bull. Math. Biol. 2019;81, 38–80.
Bruna M, Breward CJW. The Influence of Non-Polar Lipids on Tear Film Dynamics. J. Fluid Mech. 2014;746, 565–605. doi: 10/f52hj5.
Stapf M, Braun R, King-Smith P. DuplexTear Film Evaporation Analysis. Bull.Math. Biol. 2017;79, 2814–2846.
Sharma A, Ruckenstein E. Mechanism of Tear Film Rupture and Formation of Dry Spots on Cornea. J. Coll. Interface Sci. 1985;106, 12–27.
Sharma A, Khanna R, Reiter G. A thin film analog of the corneal mucus layer of the tear film: an enigmatic long range non-classical DLVO interaction in the breakup of thin polymer films. Coll. Surf. B, 1999;14, 223–35.
Dey M, Vivek AS, Dixit HN, Richhariya A, Feng JJ. A model of tear-film breakup with continuous mucin concentration and viscosity profiles. J. Fluid Mech. 2019;858, 352–376. doi: 10.1017/jfm.2018.776.
Dey M, Vivek AS, Dixit HN, Richhariya A, Feng JJ. A model of tear-film breakup with continuous mucin concentration and viscosity profiles–CORRIGENDUM. J. Fluid Mech. 2020;889, E1. doi: 10.1017/jfm.2020.138.
Choudhury A, Dey M, Dixit HN, Feng JJ. Tear-film breakup: The role of membrane-associated mucin polymers. Phys. Rev. E, 2021;103, 013018. doi: 10.1103/PhysRevE.103.013108.
Jones MB, Please CP, McElwain DLS, Fulford GR, Roberts AP, Collins MJ. Dynamics of Tear Film Deposition and Drainage. Bull. Math. Biol. 2005;22, 265–288.
Jones MB, McElwain DLS, Fulford GR, Collins MJ, Roberts AP. The Effect of the Lipid Layer on Tear Film Behavior. Bull. Math. Biol. 2006;68, 1355–1381. doi: 10/b73dc8.
Aydemir E, Breward CJW, Witelski TP. The Effect of Polar Lipids on Tear Film Dynamics. Bull Math Biol, 2011;73(6): 1171–1201. doi: 10/c2brfd.
Maki KL, Braun RJ, Barron GA. The influence of a lipid reservoir on the tear film formation. Math. Med. Biol. 2020;37, 364–389. doi: 10.1093/imammb/dqz018.
Heryudono A, BraunRJ, Driscoll TA, Maki KL, Cook LP, King-Smith PE. Single-Equation Models for the Tear Film in a Blink Cycle: Realistic Lid Motion. Math. Med. Biol. 2007;24(4): 347–377. doi: 10/ccnp9j.
Deng Q, Braun RJ, Driscoll TA, King-Smith PE. A Model for the Tear Film and Ocular Surface Temperature for Partial Blinks. Interfacial Phen Heat. Trans. 2013;1(4): 357–381. doi: 10.1615/interfacphenomheattransfer.v1.i4.40.
Zubkov VS, Breward CJ, Gaffney EA. Coupling fluid and solute dynamics within the ocular surface tear film: a modelling study of black line osmolarity. Bull. Math. Biol. 2012;74, 2062–2093.
Allouche M, Abderrahmane HA, Djouadi SM, Mansouri K. Influence of curvature on tear film dynamics. Euro. J. Mech. B Fluids, 2017;66, 81–91.
Jossic L, Lefevre P, de Loubens C, Magnin A, Corre C. The Fluid Mechanics of Shear-Thinning Tear Substitutes. J. Non-Newtonian Fluid Mech. 2009;161, 1–9. doi: 10/cpjkfv.
Mehdaoui H, Ait Abderrahmane H, Nait Bouda F, Koulali A, Hamani S. 2D numerical simulation of tear film dynamics: Effects of shear-thinning properties. Euro. J. Mech. B Fluids, 2021; 128–136.
Mehdaoui H, Ait Abderrahmane H, de Loubens C, Nait Bouda F, Hamani S. Dynamics of a Gel-Based Artificial Tear Film with an Emphasis on Dry Disease Treatment Applications. Gels, 2021;7, 215. doi: 10.3390/gels7040215.
Maki KL, Braun RJ, Ucciferro P, Henshaw WD, King-Smith PE. Tear Film Dynamics on an Eye-Shaped Domain. Part 2. Flux Boundary Conditions. J. Fluid Mech. 2010;647, 361–390. doi: 10.1017/s002211200999382x.
Li L.and Braun RJ, Driscoll TA, Henshaw WD, Banks JW, King-Smith PE. Computed Tear Film and Osmolarity Dynamics on an Eye-Shaped Domain. Math. Med. Biol. 2016;33, 123–157. doi: 10/gf3mw9.
Li L, Braun RJ, Henshaw WD, King-Smith PE. Computed flow and fluorescence over the ocular surface. Math. Med. Biol. 2018;35, 51–85.
Brosch JK, Driscoll TA, Braun RJ. Simulation of Thin Film Equations on an Eye-Shaped Domain with Moving Boundary. APS March Meeting Abstracts. 2016;
Braun RJ, Driscoll TA, Begley CG. Mathematical Models of the Tear Film. Mathematical Modeling of Ocular Fluid Dynamics: From Theory to Clinical Applications. Springer-Birkhauser, 2019; 387–432.
Maki KL, Henshaw WD, McManus A, Braun RJ, Chapp DM, Driscoll TA. A Model for Tear Film Dynamics during a Realistic Blink. J. Modeling Ophthalmol. 2019;3, 21–27. doi: 10.35119/maio.v2i3.91.
Li L, Braun RJ, Maki KL, Henshaw WD, King-Smith PE. Tear Film Dynamics with Evaporation, Wetting and Time-Dependent Flux Boundary Condition on an Eye-Shaped Domain. Phys. Fluids. 2014;26, 052101.
Braun RJ. Dynamics of the Tear Film. Annu. Rev. Fluid Mech. 2012;44(1): 267–297. doi: 10 .1146 /annurev-fluid-120710-101042.
Zhong L, Ketelaar CF, Braun RJ, Begley CG, King-Smith PE. Mathematical Modelling of Glob-Driven Tear Film Breakup. Math. Med. Biol. 2018;36(1): 55–91. doi: 10/gf3mxc.
Luke RA, Braun RJ, Driscoll TA, Awisi-Gyau D, Begley CG. Parameter Estimation for Mixed-Mechanism Tear Film Thinning. Bull. Math. Biol. 2021;83(5): 56. doi: 10/gmq9gp.
Luke RA, Braun RJ, Begley CG. Mechanistic determination of tear film thinning via fitting simplified models to tear breakup. Modeling Artif. Intel. Ophthalmol. 1 2021;3, 71–100. doi: 10.35119/maio.v3i1.114.
Luke RA, Braun RJ, Driscoll TA, Begley CG, Awisi-Gyau D. Parameter Estimation for Evaporation-Driven Tear Film Thinning. Bull. Math. Biol. 2020;82(6): 71. doi: 10.1007/s11538-020-00745-8.
NB Carlson, D Kurtz, eds. Clinical Procedures for Ocular Examination. 3rd ed. NewYork: McGraw-Hill, Medical Pub. Div, 2004;
Webber WRS, Jones DP. Continuous Fluorophotometric Method Measuring Tear Turnover Rate in Humans and Analysis of Factors Affecting Accuracy. Med. Biol. Eng. Comput. 1986;24, 386–392.
He K, Zhang X, Ren S, Sun J. Deep Residual Learning for Image Recognition. 2016 IEEE Conference on Computer Vision and Pattern Recognition (CVPR). Las Vegas, NV, USA: IEEE, 2016; 770–778. doi: 10.1109/CVPR.2016.90.
Higham CF, Higham DJ. Deep Learning: An Introduction for Applied Mathematicians. SIAM Review, 2019;61(3): 860–891. doi: 10/ggchj6.
Driscoll T, Braun RJ, Begley CG. Automatic Detection of the Cornea Location in Video Captures of Fluorescence. Modeling Artif. Intel. Ophthalmol. 2021;3(1): 55–70. doi: 10/gmwmgg.
Nichols JJ, King-Smith PE, Hinel EA, Thangavelu M, Nichols KK. The use of fluorescent quenching in studying the contribution of evaporation to tear thinning. Invest. Ophthalmol. Vis. Sci. 2012;53(9): 5426–5432.
Braun RJ, Gewecke NR, Begley CG, King-Smith PE, Siddique JI. A model for tear film thinning with osmolarity and fluorescein. Invest. Ophthalmol. Vis. Sci. 2014;55, 1133–1142. doi: 10.1167/iovs.13-12773.
Wu Z, Begley CG, Port N, Bradley A, Braun R, King-Smith E. The Effects of Increasing Ocular Surface Stimulation on Blinking and Tear Secretion. Invest. Ophthalmol. Vis. Sci. 2015;56, 4211–4220. doi: 10.1167/iovs.14-16313.
Creech J, Do LT, Fatt I, Radke C. In vivo tear-film thickness determination and implications for tear film stability. Curr. Eye Res. 1998;17(11): 1058–1066. doi: 10.1076/ceyr.17.11.1058.5233.
Wang J, Fonn D, Simpson TL, Jones L. Precorneal and pre- and postlens tear film thicknessmeasured indirectly with optical coherence tomography. Invest. Ophthalmol. Vis. Sci. 2003;44, 2524–2528.
Tomlinson A, Khanal S, Ramaesh K, Diaper C, McFadyen A. Tear Film Osmolarity: Determination of a Referent for Dry Eye Diagnosis. Invest. Ophthalmol. Vis. Sci. 2006;47(10): 4309–4315. ISSN: 1552-5783. doi: 10.1167/iovs.05-1504.
Jacobi C, Jacobi A, Kruse FE, Cursiefen C. Tear Film Osmolarity Measurements in Dry Eye Disease Using Electrical Impedance Technology. Cornea, 2011;30(12): 1289. ISSN: 0277-3740. doi: 10.1097/ICO.0b013e31821de383.
Gilbard JP, Farris RL, Santamaria J. Osmolarity of tear microvolumes in keratoconjunctivitis sicca. Arch. Ophthalmol. 1978;96(4): 677–681.
Lemp MA, Bron AJ, Baudouin C, Benítez del Castillo JM, Geffen D, Tauber J, et al. Tear Osmolarity in the Diagnosis and Management of Dry Eye Disease. Amer. J. Ophthalmol. 2011;151(5): 792–798.e1. ISSN: 0002-9394. doi: 10.1016/j.ajo.2010.10.032.
Versura P, Profazio V, Campos EC. Performance of Tear Osmolarity Compared to Previous Diagnostic Tests for Dry Eye Diseases. Curr. Eye Res. 2010;35(7): 553–564. ISSN: 0271-3683. doi: 10 .3109/02713683.2010.484557.
Mengher LS, Bron AJ, Tonge SR, Gilbert DJ. Effect of Fluorescein Instillation on the Pre-corneal Tear Film Stability. Curr. Eye Res. 1985;4, 9–12.
Cho P, Douthwaite W. The relation between invasive and noninvasive tear break-up time. Optom. Vis. Sci. 1995;72, 17–22.
Mooi JK, Wang MTM, Lim J, Müller A, Craig JP. Minimising instilled volume reduces the impact of fluorescein on clinical measurements of tear film stability. Cont. Lens Ant. Eye, 3 2017;40, 170–174. doi: 10.1016/j.clae.2017.01.004.
Cox SM, Nichols KK, Nichols JJ. Agreement between Automated and Traditional Measures of Tear Film Breakup. Optom Vis Sci. 9 2015;92, e257–e263. doi: 10.1097/OPX.0000000000000648.
Paugh JR, Tse J, Nguyen T, Sasai A, Chen E, Jesus MT de, et al. Efficacy of the Fluorescein Tear Breakup Time Test in Dry Eye. Cornea, 1 2019;39, 92–98.
Speakman S, Wang MTM, Muntz A, Vidal-Rohr M, Menduni F, Dhallu S, et al. Investigating the diagnostic utility of non-invasive tear film stability and breakup parameters: A prospective diagnostic accuracy study. Clin. Exp. Optom. 2022;25, 72–74. doi: 10.1016/j.jtos.2022.04.006.
Bai Y, Ngo W, Khanal S, Nichols J. Characterization of the thickness of the Tear Film Lipid Layer in Meibomian Gland Dysfunction using high resolution optical microscopy. Ocul. Surf. 2022;24, 34–39. doi: https://doi.org/10.1016/j.jtos.2021.12.011.
Belmonte C, Nichols J, Cox S, Brock J, Begley C, Bereiter D, et al. TFOS DEWS II Pain and Sensation Report. Ocul Surf, 2017;15, 404–437.
Parra A, Gonzalez-Gonzalez O, Gallar J, Belmonte C. Tear fluid hyperosmolality increases nerve impulse activity of cold thermoreceptor endings of the cornea. Pain, 2014;155, 1481–1491.
Hirata H,Rosenblatt MI. Hyperosmolar tears enhance cooling sensitivity of the corneal nerves in rats: possible neuralbasis for cold-induced dry eyepain. Invest. Ophthalmol. Vis. Sci. 2014;55, 5821–5833.
Situ P, Begley CG, Simpson TL. Effects of Tear Film Instability on Sensory Responses to Corneal Cold, Mechanical, and Chemical Stimuli. Invest. Ophthalmol. Vis. Sci. 2019;60, 2935–2941.
Belmonte C. Pain, Dryness, and Itch Sensations in Eye Surface Disorders Are Defined By a Balance Between Inflammation and Sensory Nerve Injury. Cornea, 2019;38 Suppl 1, S11–S24.
Li W, Lin MC. Pain Sensitivity Associated With the Length of the Maximum Interblink Period. Invest. Ophthalmol. Vis. Sci. 2018;59, 238–245. doi: 10.1167/iovs.17-22950.
Mota MC, Carvalho P, Ramalho J, Leite E. Spectrophotometric analysis of sodium fluorescein aqueous solutions. Determination of molar absorption coefficient. Intl. Ophthalmol. 1991;15(5): 321–326.
Tiffany JM. The viscosity of human tears. Intl. Ophthalmol. 1991;15(6): 371–376.
Nagyová B, Tiffany JM. Components responsible for the surface tension of human tears. Curr. Eye Res. 1999;19(1): 4–11.