Keywords
Abstract
Intraocular pressure (IOP), arterial blood pressure (PA), and cerebrospinal fluid (CSF) pressure have been identified as major players in several ocular pathologies, including glaucoma, central vein occlusion, and papilledema, to name a few. IOP, PA, and CSF pressures are not independent from each other. For example, aqueous humor and CSF flows, whose mechanics contribute to establish IOP and CSF pressure levels, originate from blood flow, which is driven by PA. As a consequence, it is difficult to experimentally isolate IOP, PA, and CSF pressure and to disentangle their effect in pathological conditions. Here we utilize a theoretical approach to address this issue.
References
Lakin WD, Stevens SA. Modelling the Response of Intracranial Pressure to Microgravity Environments. Aspects of Mathematical Modelling. Springer, 2008;211–227.
Guidoboni G, Harris A, Cassani S, et al. Intraocular pressure, blood pressure, and retinal blood flow autoregulation: a mathematical model to clarify their relationship and clinical relevance. Invest Ophthalmol Vis Sci. 2014;55(7):4105–4118.
Kiel JW, Hollingsworth M, Rao R, Chen M, Reitsamer HA. Ciliary blood flow and aqueous humor production. Prog Retin Eye Res. 2011;30(1):1–17.
Szopos M, Cassani S, Guidoboni G, et al. Mathematical modeling of aqueous humor flow and intraocular pressure under uncertainty: towards individualized glaucoma management. Journal for Modeling in Ophthalmology. 2016;1(2):29–39.
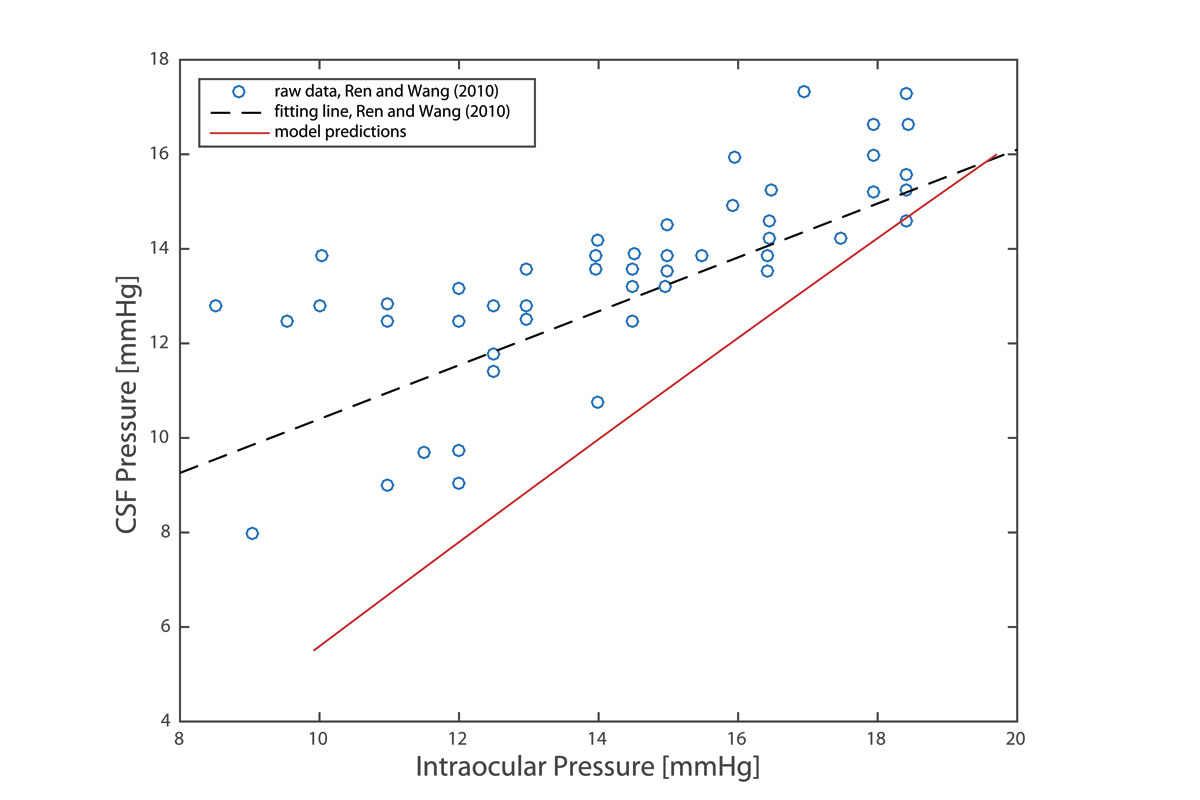
Ren R, Jonas JB, Tian G, et al. Cerebrospinal fluid pressure in glaucoma: a prospective study. Ophthalmology, 2010;117(2): 259–266.
Bill A. The uveal venous pressure. Arch Ophthalmol. 1963;69(6):780–782.
Dielemans I, Vingerling JR, Algra D, Hofman A, Grobbee DE, de Jong PT. Primary open-angle glaucoma, intraocular pressure, and systemic blood pressure in the general elderly population: the Rotterdam Study. Ophthalmology. 1995;102(1):54–60.
Mitchell P, Lee AJ,Wang JJ, Rochtchina E. Intraocular pressure over the clinical range of blood pressure: Blue Mountains Eye Study findings. Am J Ophthalmol. 2005;140(1):131–132.
XuL,Wang H,Wang Y, Jonas JB. Intraocular pressure correlated with arterial blood pressure: the Beijing Eye Study. Am. J. Ophthalmol. 2007;144(3):461–462.