Keywords
Abstract
Purpose: The aim of this study was to compare costs related to glaucoma treatment for early- and moderate-stage glaucoma patients.
Design: Descriptive observational study.
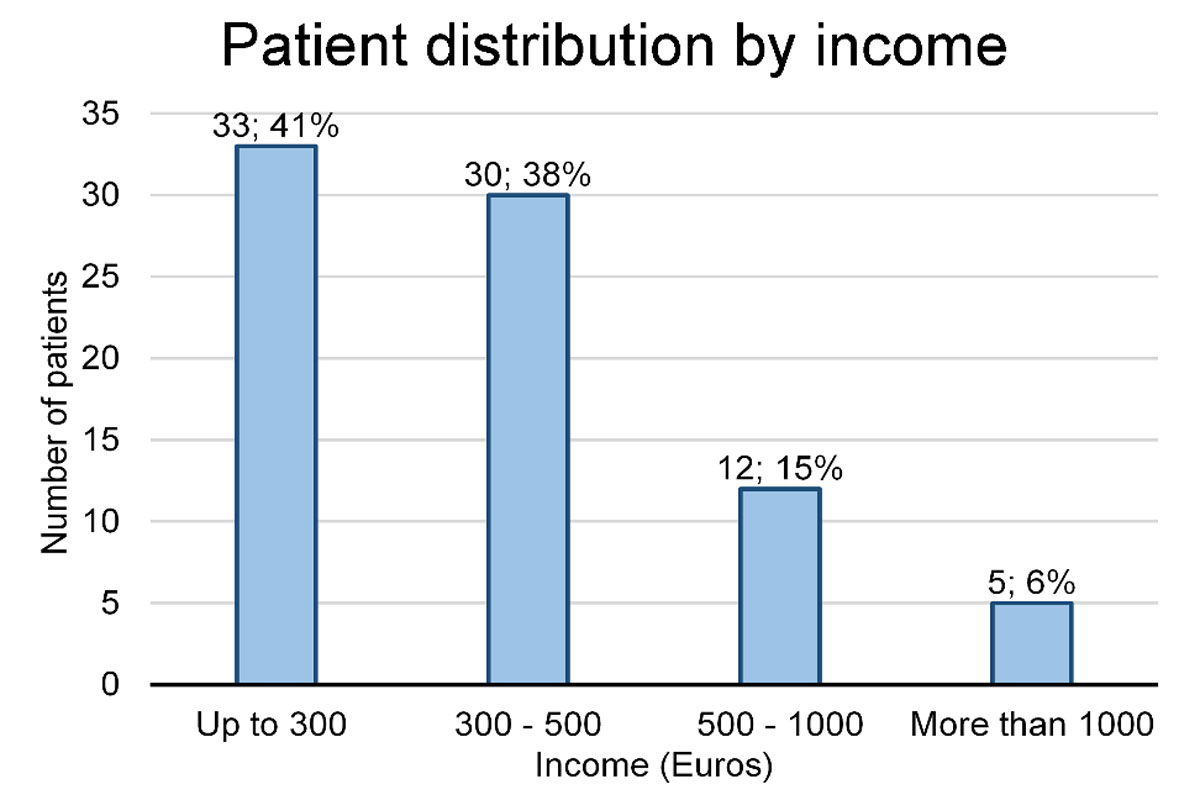
Methods: The study was conducted at the Eye Clinic in the Hospital of the Lithuanian University of Health Sciences Kauno Klinikos in Lithuania. An original questionnaire was administered to 80 open-angle glaucoma patients. Data regarding the age, gender, living area, occupation, income, concomitant diseases, frequency of outpatient visits, use of topical antiglaucoma and other medications, treatment and transportation costs were collected. The Hodapp classification was used to divide patients into two main groups of early- and moderate-stage glaucoma according to visual field loss. Results with p < 0.05 were interpreted as statically significant.
Results: There were 37 patients with early-stage glaucoma and 43 patients with moderate glaucoma. Moderate-stage glaucoma patients were 73 (± 8) years old, while patients with early-stage glaucoma were 63 (± 11) years old, (p < 0.001). Early-stage glaucoma patients visited their ophthalmologist 2.5 (± 1.5) times per year, while patients with moderate glaucoma had 4.4 (± 2.7) outpatient visits per year (p < 0.001). Patients with early-stage glaucoma used 1.8 (± 0.9) medications, while patients with moderate glaucoma used 2.9 (± 0.9) medications (p < 0.001). Combined costs for treatment and transportation totaled an average of 4.7% of patient income. Patients that were in the early stages of glaucoma spent about 3.2% of their annual income for glaucoma care and transportation, while patients with moderate-stage glaucoma spent about 5.9% of their income (p = 0.003).
Conclusion: Moderate-stage glaucoma patients had significantly higher expenses related to glaucoma than early-stage glaucoma patients. Costs related to glaucoma comprised a significantly greater part of the income of patients who were retired than patients who were employed.
References
Cohen LP, Pasquale LR. Clinical characteristics and current treatment of glaucoma. Cold Spring Harb Perspect Med. 2014;4(6):a017236. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4031956/
Weinreb R, Aung T, Medeiros F. The pathophysiology and treatment of glaucoma. JAMA. 2014;311(18):1901. doi:10.1001/jama.2014.3192
Foster A, Resnikoff S. The impact of Vision 2020 on global blindness. Eye (Lond). 2005;19(10):1133–1135. doi:10.1038/sj.eye.6701973
Bourne RRA, Jonas JB, Flaxman SR, et al. Prevalence and causes of vision loss in high-income countries and in Eastern and Central Europe: 1990–2010. Br J Ophthalmol. 2014;12;98(5):629 LP-638. Available from: http://bjo.bmj.com/content/98/5/629.abstract
Varma R, Lee PP, Goldberg I, Kotak S. an assessment of the health and economic burdens of glaucoma. Am J Ophthalmol. 2011;152(4):515–522. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3206636/
Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262–7. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1856963/
Leite MT, Sakata LM, Medeiros FA. Managing glaucoma in developing countries. Arq Bras Oftalmol. 2011;74(2):83–84. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3787827/
Bettin P, Di Matteo F. Glaucoma: present challenges and future trends. Ophthalmic Res. 2013;50(4):197–208. Available from: http://www.karger.com/DOI/10.1159/000348736
Buys YM, Gaspo R, Kwok K. Referral source, symptoms, and severity at diagnosis of ocular hypertension or open-angle glaucoma in various practices. Can J Ophthalmol. 2017;47(3):217–222. doi:10.1016/j.jcjo.2012.03.031
Boland MV, Ervin AM, Friedman DS, et al. Comparative effectiveness of treatments for open-angle glaucoma: a systematic review for the US Preventive Services Task Force. Ann Intern Med. 2013;158(4):271-279.
Stewart WC, Konstas AG, Nelson LA, Kruft B. Meta-analysis of 24-hour intraocular pressure studies evaluating the efficacy of glaucoma medicines. Ophthalmology. 2008;115(7):1117e1-1122e1
Waldock A, Snape J, Graham C. Effects of glaucoma medications on the cardiorespiratory and intraocular pressure status of newly diagnosed glaucoma patients. Br J Ophthalmol. 2000;84(7):710–713. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1723530/
Kumbar SK, Mirje M, Moharir G, Bharatha A. Cost analysis of commonly used combination of drugs in primary open angle glaucoma. J Clin Diagn Res. 2015;9(5):FC05-FC08. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4484082/
Lorenz K, Wolfram C, Breitscheidel L, Shlaen M, Verboven Y, Pfeiffer N. Direct cost and predictive factors for treatment in patients with ocular hypertension or early, moderate and advanced primary open-angle glaucoma: the CoGIS study in Germany. Graefe’s Arch Clin Exp Ophthalmol. 2013;251(8):2019–2028. doi:10.1007/s00417-013-2354-z
Traverso CE, Walt JG, Kelly SP, et al. Direct costs of glaucoma and severity of the disease: a multinational long term study of resource utilisation in Europe. Br J Ophthalmol. 2005 89(10):1245–1249. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1772870/
Goldberg I. Stepping up glaucoma management: when and how? Open Ophthalmol J. 2009;3:67–69. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2760861/
Gaidelytė R, Garbuvienė M, Madeikytė N. Lithuanian Ministry of Health Health Information Centre of Institute of Hygiene Health Statistics of Lithuania 2015; Available from: www.hi.lt
National Health Insurance Fund under The Ministry of Health. Healthcare in Lithuania. Vlk.lt. http://www.vlk.lt/sites/en/healthcare-in-lithuania/. Published 2019
Susanna R Jr, Vessani RM. Staging glaucoma patient: why and how?. Open Ophthalmol J. 2009;3:59–64. 2009. doi:10.2174/1874364100903020059
Elze T, Pasquale LR, Shen LQ, Chen TC, Wiggs JL, Bex PJ. Patterns of functional vision loss in glaucoma determined with archetypal analysis. J R Soc Interface. 2014;12(103):20141118–20141118. doi:10.1098/rsif.2014.1118
Sharma A, Jofre-Bonet M, Panca M, Lawrenson JG, Murdoch I. Hospital-based glaucoma clinics: what are the costs to patients. Eye. 2010;24(6):999–1005. doi:10.1038/eye.2009.284
Heijl A. Concept and importance of visual field measurements to detect glaucoma progression. Glaucoma now. 2010;(2):2–4.
Lee PP, Walt JG, Doyle JJ, et al. A multicenter, retrospective pilot study of resource use and costs associated with severity of disease in glaucoma. Arch Ophthalmol. 2006;124(1):12–19. doi:10.1001/archopht.124.1.12
Schmier JK, Halpern MT JM. The economic implications of glaucoma: A literature review. Pharmacoeconomics. 2007;(25):287–308.
Vaahtoranta-Lehtonen H, Tuulonen A, Aronen P et al. Cost effectiveness and cost utility of organized screening programme for glaucoma. Acta Ophthalmol Scand. 2007;(85):508–518.
Tuulonen A. Challenges of glaucoma care – high volume, high quality, low cost. Acta Ophthalmol. 2013;91(1):3–5. doi:10.1111/aos.12088
Hagman J. Comparison of resource utilization in the treatment of open-angle glaucoma between two cities in Finland: is more better? Acta Ophthalmol. 2013;91(thesis3):1–47. doi:10.1111/aos.12141
Lindblom B, Nordmann J-P, Sellem E, et al. A multicentre, retrospective study of resource utilization and costs associated with glaucoma management in France and Sweden. Acta Ophthalmol Scand. 2005;84(1):74–83. doi:10.1111/j.1600-0420.2005.00560.x
OECD Statistics. Stats.oecd.org. 2017 [Internet]. Available from: https://stats.oecd.org/
Statistics Lithuania. Labour Market Yearbook 2016. Average net monthly earnings, 2006–2016. Vilnius, Lithuania; 2017. Available from: https://osp.stat.gov.lt/services-portlet/pub-edition-file?id=27544
Statistics Lithuania. Social Protection in Lithuania 2015. Average monthly state social insurance pension, 2010–2015. Lithuania, Vilnius; 2016. Available from: https://osp.stat.gov.lt/statistikos-leidiniu-katalogas?publication=25060
Olsen J, Berdeaux G, Skov J. Glaucoma costs in Denmark in treatment naive patients. Acta Ophthalmol. 2013;91(1):25–31. doi:10.1111/j.1755-3768.2011.02212.x
Olthoff C M, Schouten J S, van de Borne B W, Webers C A. Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension: an evidence-based review. Ophthalmology 2004;112(6): 953-961.
Luca Rossetti OSP. Treatment strategies to help prevent progression. Glaucoma Now. 2010;(2):8–9.